In prior blogs, I’ve written about the need for our heatlh care system to tear down the silos. One area of this is the use of health risk and social/behavioral assessments - what Sustainable Health Systems calls health ecology. There is lots of good activity going on in these domains, but it’s as if nobody is looking from the 40,000 foot view, and particularly not with the view of how the pieces will fit together when it’s all done.
Conspiracy theorists would say vested interests are preserving their stakes, but at 57 I’ve seen enough of the world works to believe that it’s just everyone doing what they know how to do. What the world really needs, though, is people who can figure out how to do something that they’ve never thought of before.
Here’s a look:
• The US Centers for Disease Control and Prevention (CDC) is promoting workforce wellness programs, in which it is common for employers to use a health risk assessment tool (HRA). Rarely is the employee’s primary care provider (PCP) asked to be involved;
• The CDC is also promoting diabetes prevention programs, though - most unfortunately - there is no well-defined business model;
• Medicare is encouraging annual wellness visits (AWV) with a PCP, in which use of an HRA is required;
• Accountable care organizations (ACOs) are also prompted by payers to use AWVs as a way of defining the PCP in health plans;
• The Institute of Medicine (IOM) and National Institutes of Health (NIH) support the inclusion of social and behavioral (health ecology) elements in the electronic health record (EHR);
• The ultimate reason for all of this is so-called “meaningful use” (popularly called meaningless use by physicians) - a belief that “big data” analytics will drive improvement in population health.
I have participated in surveys that asked if more effort (i.e., money) should be spent on getting more physicians using EHRs. My reaction was that spending money on information technology is de facto evidence that society thinks the need for data is more important than the needs of people. Every dollar spent on data is a dollar not spent on prenatal care, child nutrition, physical education, band and other character-building programs for youth that provide protectiion against the risks from exposer to sex, drugs, violence, tobacco, social strife - all from the very same socio-behavioral list of data that the IOM and NIH say needs to be collected. Do we want the data, or do we want to invest in programs that reduce risk?
Having been trained as a physician-scientist, I ‘get it’ that one needs the data to do the objective analyses that show if a program is working. But in recent years lots of money has been spent on health information technology while many patients languish in need.
In sum, my own perspective from 40,000 feet is that we’re working towards the Belief that analytics will solve the health care cost crisis, and recapture part of the economy being spent on health care. Truthfully, I share hope that we can improve everyone’s health. But as a physician I have looked into the chaos of patients lives, and think a Belief that analytics will solve our problems is a false dream. Nature is inconceivably complex beyond our comprehension, every patient’s life is a unique manifestation of thereof, shaped by the very evolutionary forces that led to life on Earth today. “Big data” analytics and treating physicians and patients as millworkers and their widgets won’t work. The chaotic variability in people’s lives means that we’re going to need fine practitioners of the ‘Art of Medicine’ for a very, very long time to come. So I won’t be the least bit surprised when the health care big data bubble bursts.
Well, then, what should we be working towards?
Population Health = Disease Burden + Health Risk
Though it should be clear by now that I’m not wearing rose-colored glasses, this formula should reveal that I really do think we need health ecology data. But at the same time, people need help more than we need this data about them. So…connect the dots! Do HRAs and AWVs, not so much to have the data but to align resources to needs. Do it to help people, not because of the analytical potential.
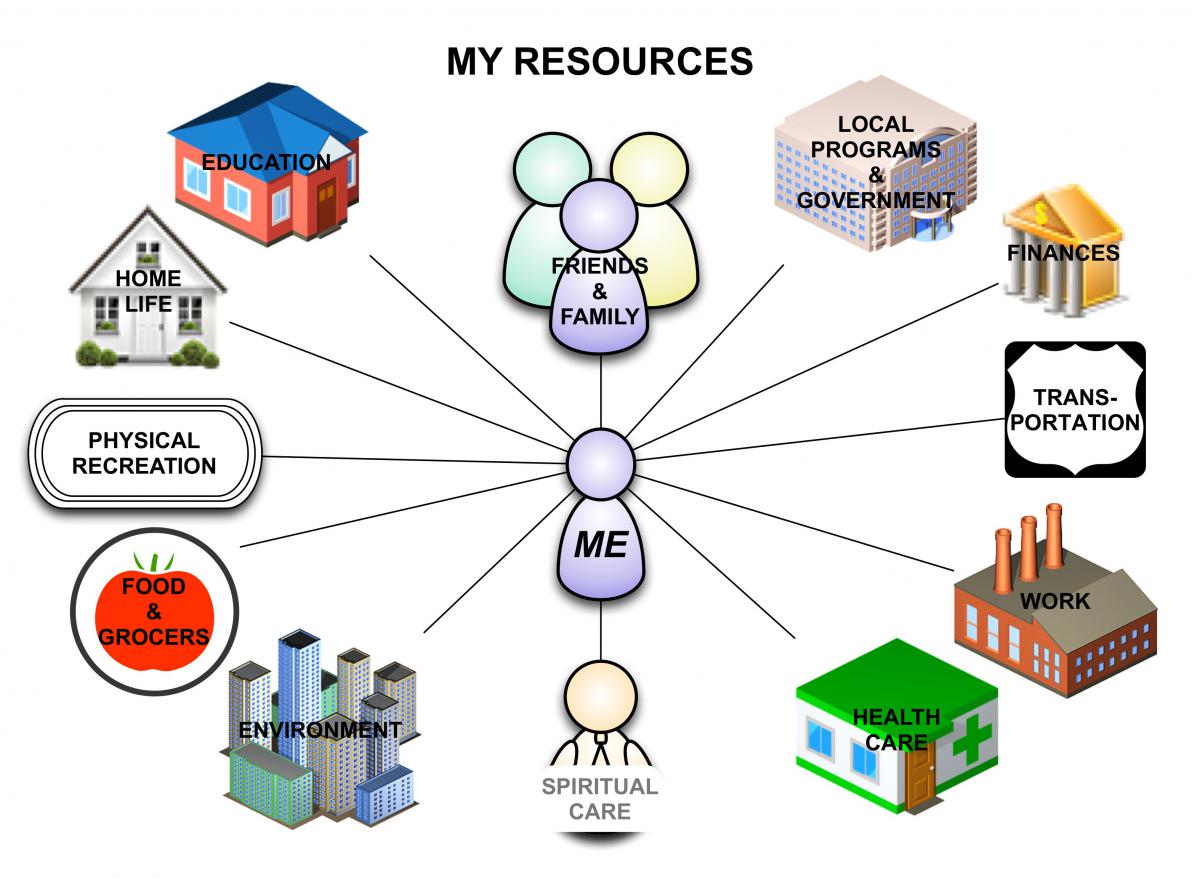
We need a collaboration between employers, PCPs and local community resources with the objective of facilitating preventive services that promote health. It makes no sense for each employer to use it’s own HRA tool, when the big data need is for PCPs to assemble this data on behalf of analytics firms (including Departments of Health)…all so that the relationships between health care expenditures, health risks and health ecology can be quantified. Put HRAs into the hands of PCPs, but do so to align community resources that empower the PCP to make referrals as part of the AWV process.
Meanwhile, create a sustainable business model for the allied health care providers who provide the resources. We don’t need diabetes prevention grants that underwrite and thereby cost-shift preventive services, we need health coaches, nutritionists, social workers, health educators and clinical exercise physiologists being paid directly for what they were trained to do - valued for their contributions to the health of society.
So if we’re going to do all of this, these allied health care staff need access to their patient’s health ecology data. They shouldn’t have to collect it again! This is why this data should not be hidden behind the EHR firewall, as the IOM and NIH suggest, but should accessible to patient-chosen resources in the community.
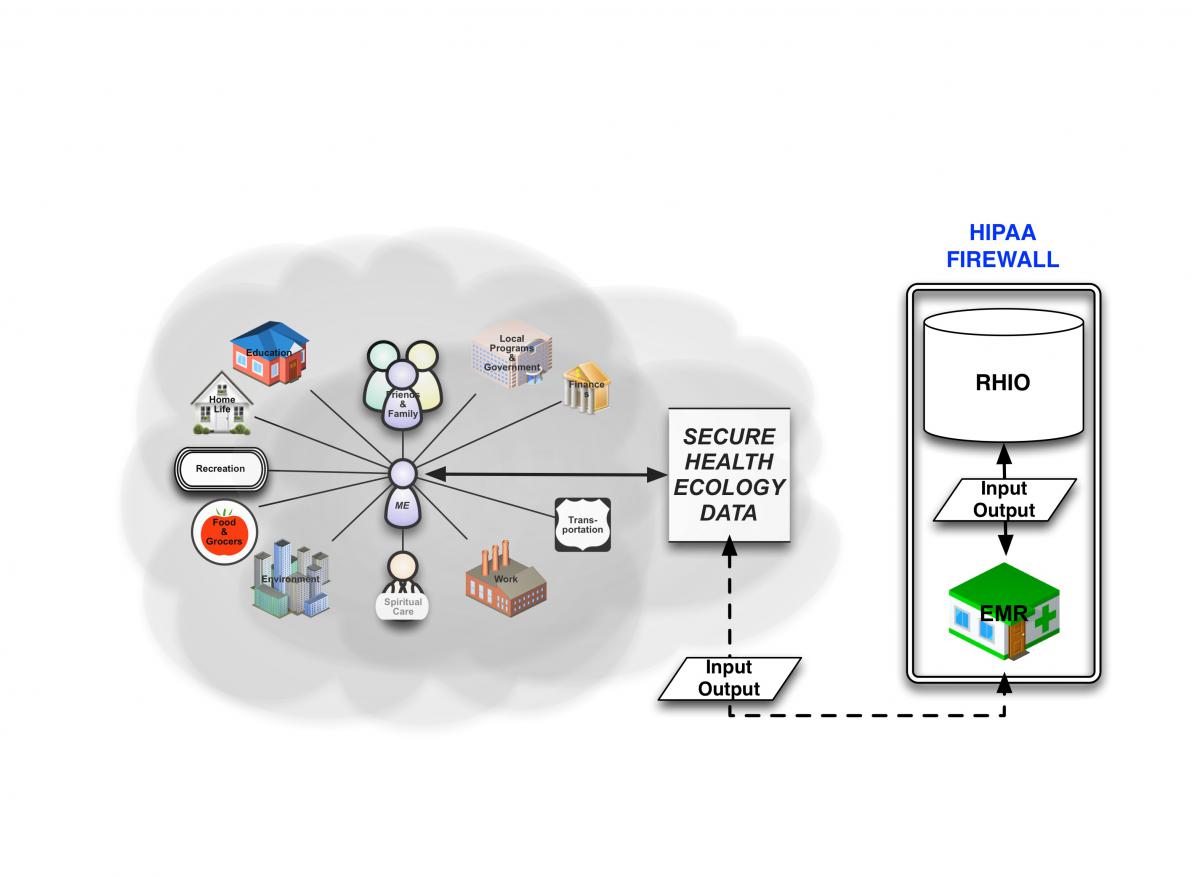
This database needs to be outside of the EHR firewall, though still a part of the PCMH, as if it were on the veranda of the medical home - open and in view to the community, but still private with access only by patient invitation.
Health ecology data needs to be fed into the EHR, but it should be imported from the patient’s-controlled database that helps them align resources to their own health risks. This model allows the PCP to provide moral imperative for addressing health promotion, while facilitating the ability of the patient to make use of appropriate resources at his or her disposal.
I can’t say it loudly enough - we must break down the walls of the public health and disease-care silos. And, for sure, we should worry far less about getting the data than about aligning resources to barriers - truly meaningful use.
- GE Moore MD's blog
- Log in to post comments
- Follow our Blog
