Diabetes is one of America’s biggest lurking health system catastrophes, which concerns us greatly at Sustainable Health Systems.
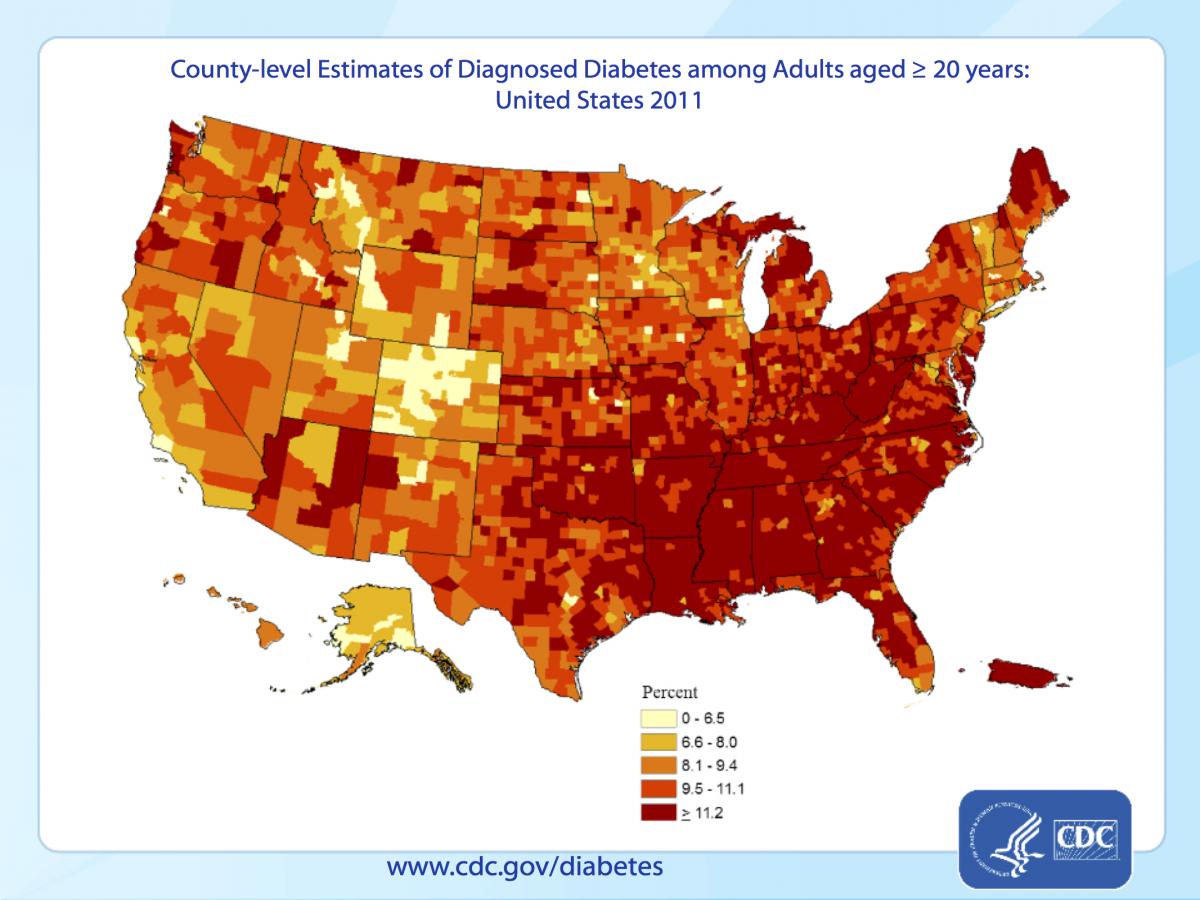
Here is the CDC (Centers for Disease Control) map of diabetes in 2011, about 95% of which is type 2 diabetes.
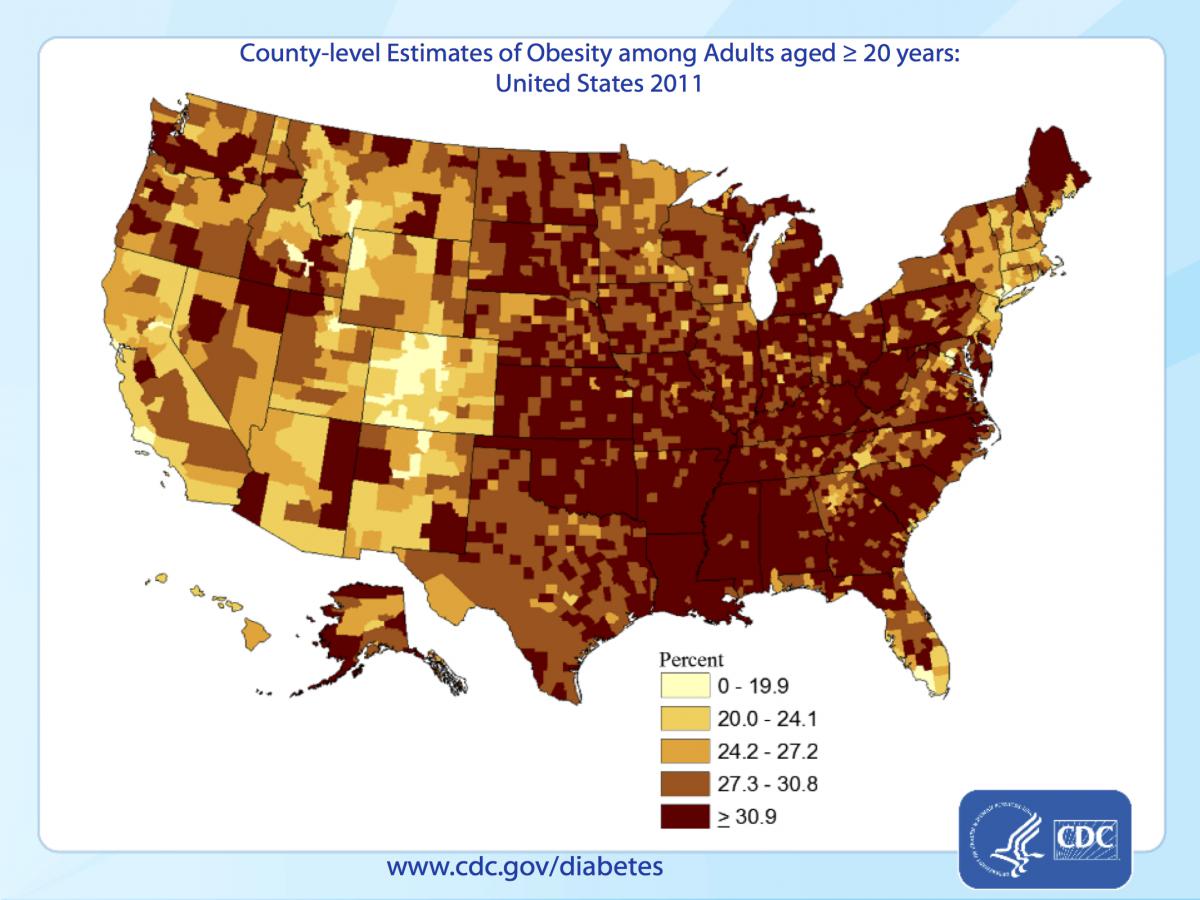
The CDC’s map of obesity, also in 2011, shows a similar pattern, though more diffuse and extending a little more broadly out from the Ohio and Mississippi basins. Obesity is important because it’s the major underlying risk factor type 2 diabetes.
The other major risk factor for type 2 diabetes is physical inactivity, and this is the CDC’s map of physical inactivity in 2011.
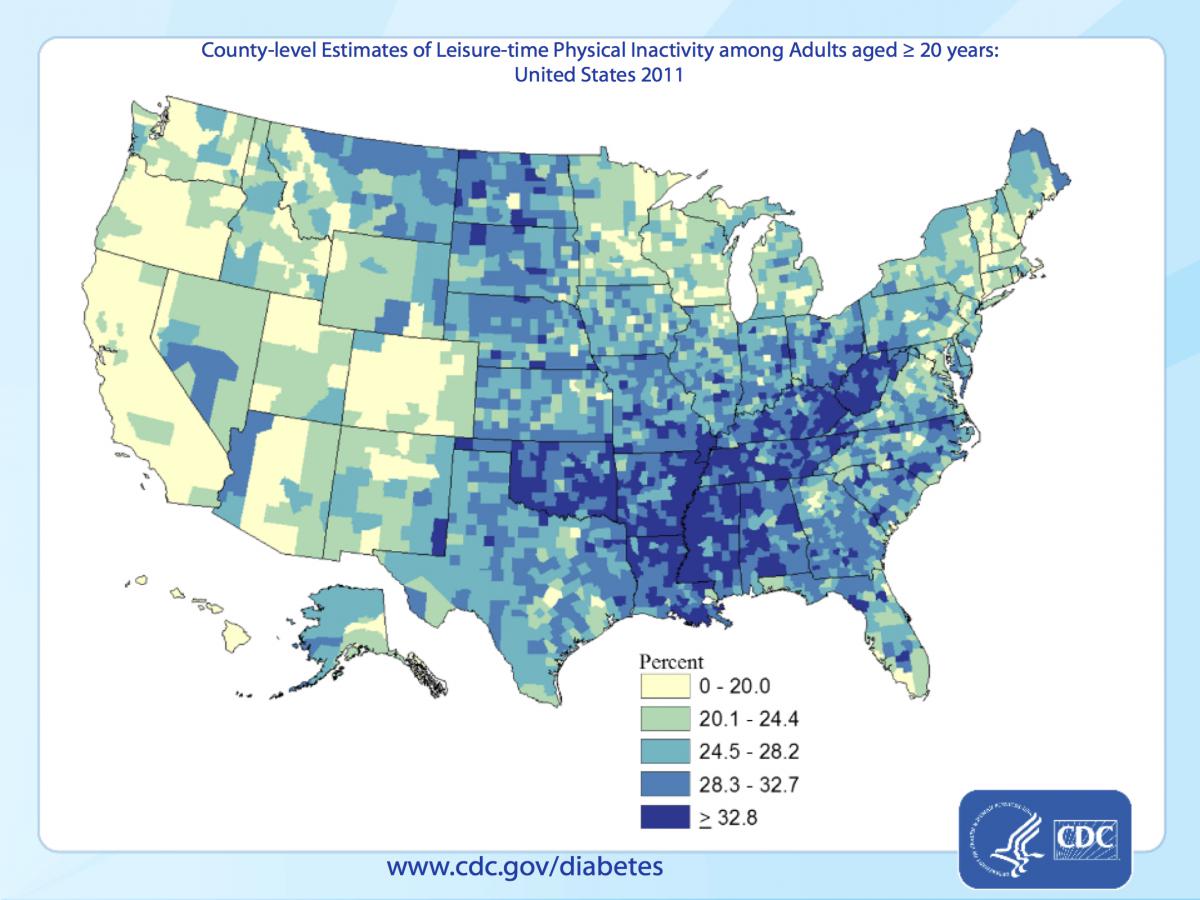
Since type 2 diabetes is largely a product of obesity and physical inactivity, it’s apparent why diabetes is focused in the southeast, Ohio and Mississippi basins, where there is a high prevalence of both sedentary lifestyle and obesity. Prevalance of inactivity and obesity are much lower on the west coast, in the mountain west and in northern New England.
Though diabetes is a non-communicable disease (meaning it’s not an infection), it has become an epidemic. Current prevalence in the USA is up to 9.3%. Among individuals who are obese and physically inactive, about 11% a year (or 1-in-9) develop type 2 diabetes every year. This puts the USA on track for nearly 13% of Americans to be diabetic by 2024.
Averting this epidemic is important for the health of our economy, because the our society spends a lot of effort and money on managing the burden of chronic disease. The CDC’s June, 2014, update from the shows that the demands of managing diabetes has become a huge burden. Costing $245 Billion a year, diabetes affects over 29 Million Americans and pre-diabetes over 100 million, ultimately leading to an enormous number of people on disability from the side-effects of diabetes. 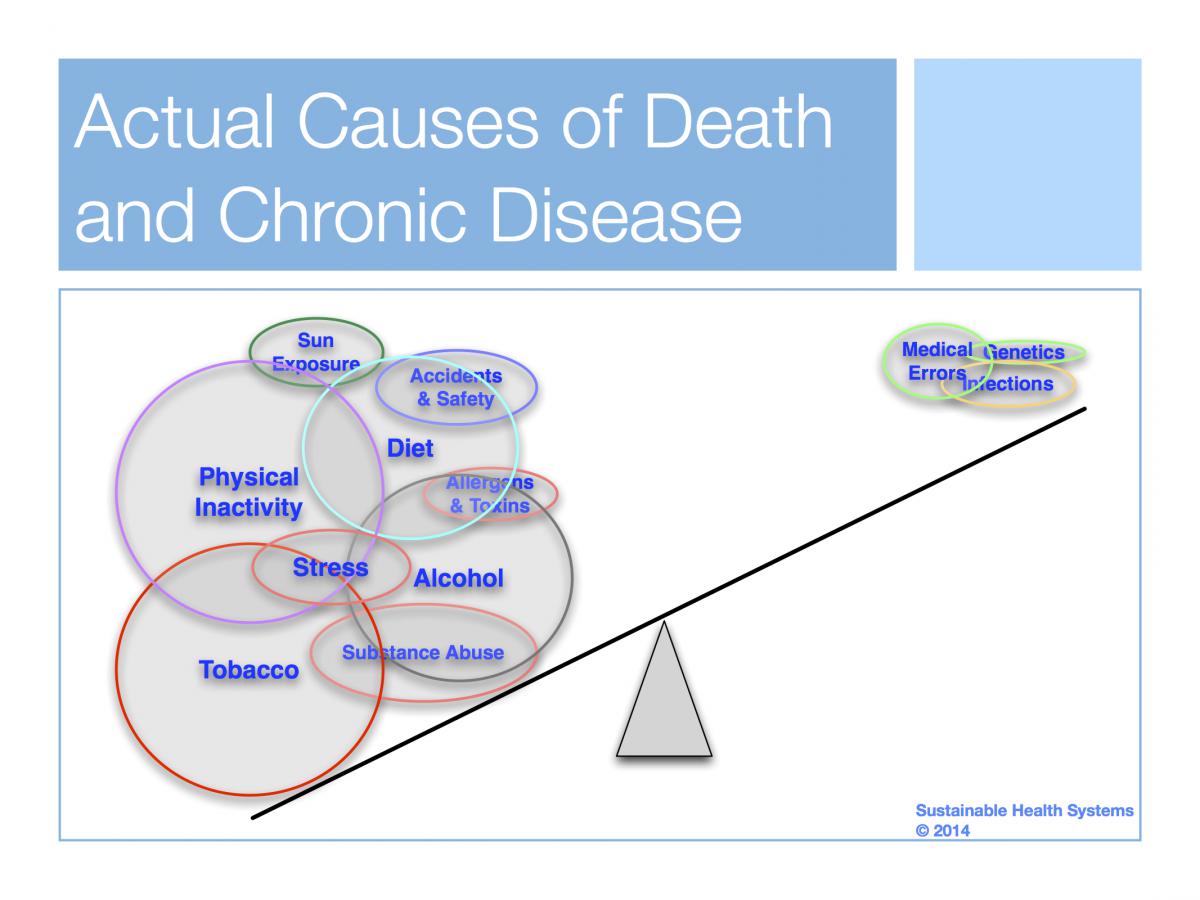
We’ve noted in prior blogs that all those efforts affect only 15% of health outcomes. The remaining 85% of health outcomes are caused by social and behavioral risk factors in a person’s life. Behaviors such as exercise.
Since it is difficult to achieve and sustain weight loss, exercise is probably the most important antidote that could avert many people from becoming diabetic.
Unfortunately, our health care system lags in addressing lack of physical activity, and does little to help people overcome ecological barriers to getting more exercise. We need more doctors prescribing exercise, but more than that we need to get people more active through programs and help from exercise professionals.
By not cutting off the fuel supply of adverse health behaviors, the fire of chronic diseases like diabetes is allowed to blaze away, unabated. Less than 10% of people with diabetes are referred to diabetes education classes, even though this is universally a covered benefit.
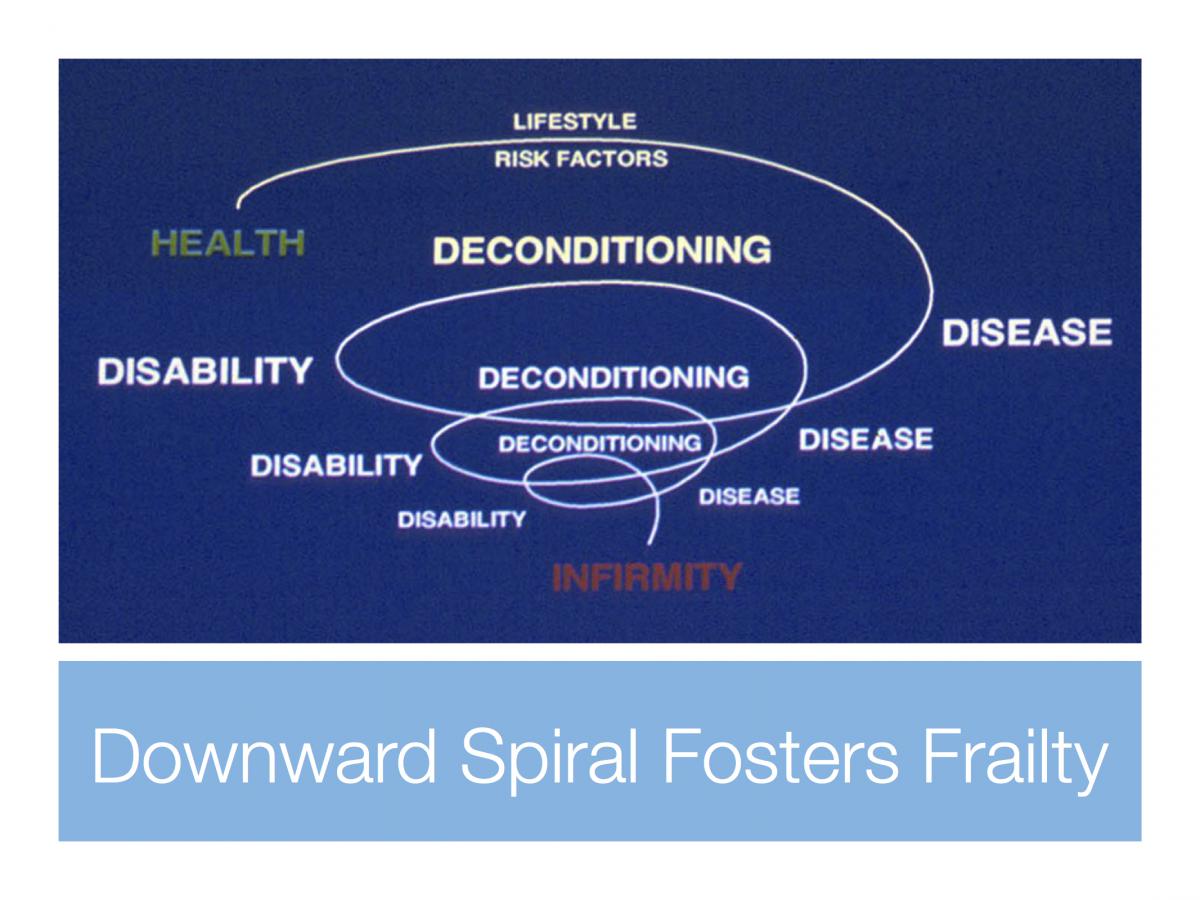
This type of failing unintentionally pushes people towards the burden of chronic disease, disability and frailty, rather than towards prolonging their vitality and well-being. Modern medicine is quite good at preventing death, so lots of people end up burdened with a chronic disease, like diabetes, trapped in a downward spiral that funnels them towards disability and frailty.
Exercise is the most important antidote to going down the spiral path of chronic disease, not just for diabetes but for many conditions. Health care networks need to do everything they can to promote physical activity and the realize that Exercise is Medicine™*.
Geoffrey E. Moore, MD FACSM
Peter G. Sepsis, MS MPH
John Sammis, MBA
Here are some resources to help:
http://exerciseismedicine.org/
http://www.physicalactivityplan.org/
* Exercise is Medicine is a Trademark owned by the American College of Sports Medicine.
- GE Moore MD's blog
- Log in to post comments
- Follow our Blog
