In the February 2024 issue of the Clinical Journal of Sports Medicine, my colleagues and I present findings from a survey conducted among sports medicine physicians in the United States, addressing the critical issue of American's lack of physical activity.[1] This project, initiated in 2019 by the American Medical Society for Sports Medicine (AMSSM), also involved leaders from both the American College of Sports Medicine (ACSM) and the American College of Lifestyle Medicine (ACLM).
Our study focused on physical activity (exercise), but underscores the importance of addressing other biopsychosocial aspects of life such as nutrition, stress management, sleep adequacy, social connectedness, and all social determinants of health. The study's main objectives were to:
• Identify profitable clinical programs that integrate exercise counseling and oversight,
• Recommend how to increase the adoption of exercise programming in medical practice, and
• Assess payer-based initiatives promoting exercise among insured clients.
Why was I asked to lead this study?
In 2003, I opened a lifestyle medicine private practice after some 16 years as a clinical investigator studying the mechanisms of exercise intolerance in chronic disease. As a new "blip on the radar" of pharmaceutical companies, I had many visits from drug reps. That my goal was to use lifestyle change to get patients OFF of medications didn’t seem to register!
A few drug reps would finish their spiel, but then have difficulty drawing away and confide that they had a Masters Degree in exercise physiology from whatever university (some of which were notable institutions, and one even had a close friend as the Chair of the department!). When I asked these reps why they were working as a drug rep, the answer was always “I couldn’t make a good living”.
Those responses were THE reason I became an exercise activist! My closest friends are exercise physiologists, I myself almost went to graduate school to get a PhD in exercise physiology. It infuriated me that exercise physiologists couldn't make a living with their training.
I got involved in ACSM’s Health and Science Policy committee, on which I served for 15 years. When Chad Carlson, a friend and colleague who was on the committee, became President-Elect of AMSSM, he asked me if I would lead this project and I agreed. Chad was in private practice, like me. He knew that I thought that the lack of a sustainable business model was a key barrier to implementation of clinical exercise services. Those drug reps had told me so.
What did our survey find?
We found that, not surprisingly, sports medicine physicians widely support exercise's therapeutic value and that they try to provide physical activity recommendations to their patients. However, many sports medicine physicians feel like they need to know more about how to prescribe exercise, and that they experience substantial-to-overwhelming challenges in the integration of exercise management services into their clinical practice. Administrative hurdles and inadequate covered benefits around exercise result in poor compensation for both physicians and exercise professionals.
My own belief is that clinical guidelines, promotion of exercise prescription from academic and professional organizations, and performance metrics like the PAVS are weak incentives and are insufficient to counter the very strong disincentive of an inadequate business model.
In America, if a doctor and/or exercise professional are to do something about a patient who is physically inactive and harming their health and well-being, those services need to be a covered benefit under the patient's health plan. Public health policies to promote physical activity aren't enough, nor is leaving it up to the patient's "personal responsibility". The vast majority of patients need help getting started.
We issue a Call to Action for 5 key issues:
1) Prioritize training in exercise and lifestyle medicine for physicians, especially in primary care settings.
2) Advocate for appropriate compensation for allied health professionals involved in exercise medicine services.
3) Remove administrative barriers hindering the promotion of physical activity.
4) Utilize allied health professionals for exercise management to optimize resource allocation.
5) Foster collaboration with employers and payers to establish sustainable models for promoting exercise, integrating incentives for both patients and healthcare providers.
What do these actions aim to achieve?
Our Call to Action aims to facilitate a paradigm shift towards proactive healthcare focused on addressing root causes of morbidity and mortality through lifestyle interventions, emphasizing the importance of physical activity.
FIGURE 1: Prevalence of Americans Meeting the 2018 Physical Activity Guidelines [2]
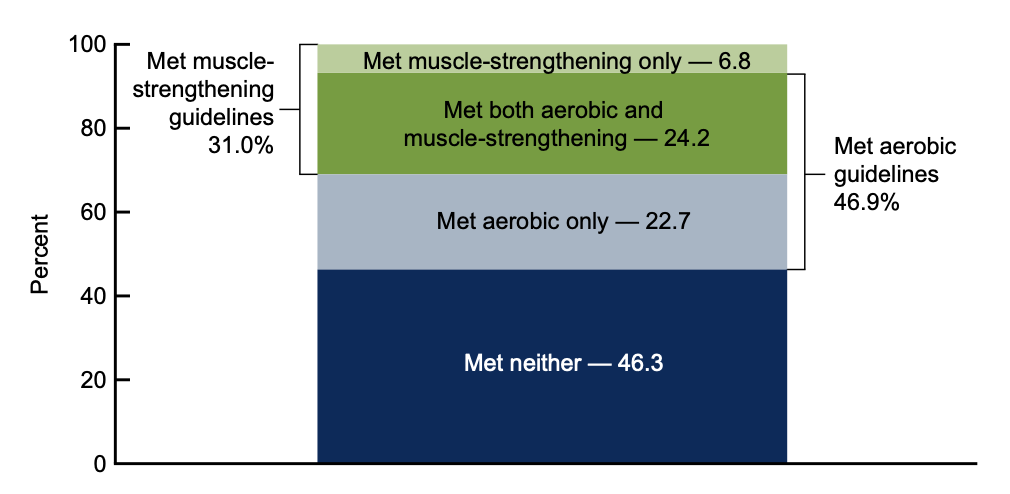
When ¾ of Americans have cardiometabolic disease or are at high risk, at a time when almost ½ of Americans don’t meet guidelines for either aerobic activity or muscle strengthening (see figure 1; note that only ¼ of Americans meet both), we can’t have exercise physiologists abandoning their chosen careers.
FIGURE 2: Causes of Death and Disability in USA, 2016 [3]
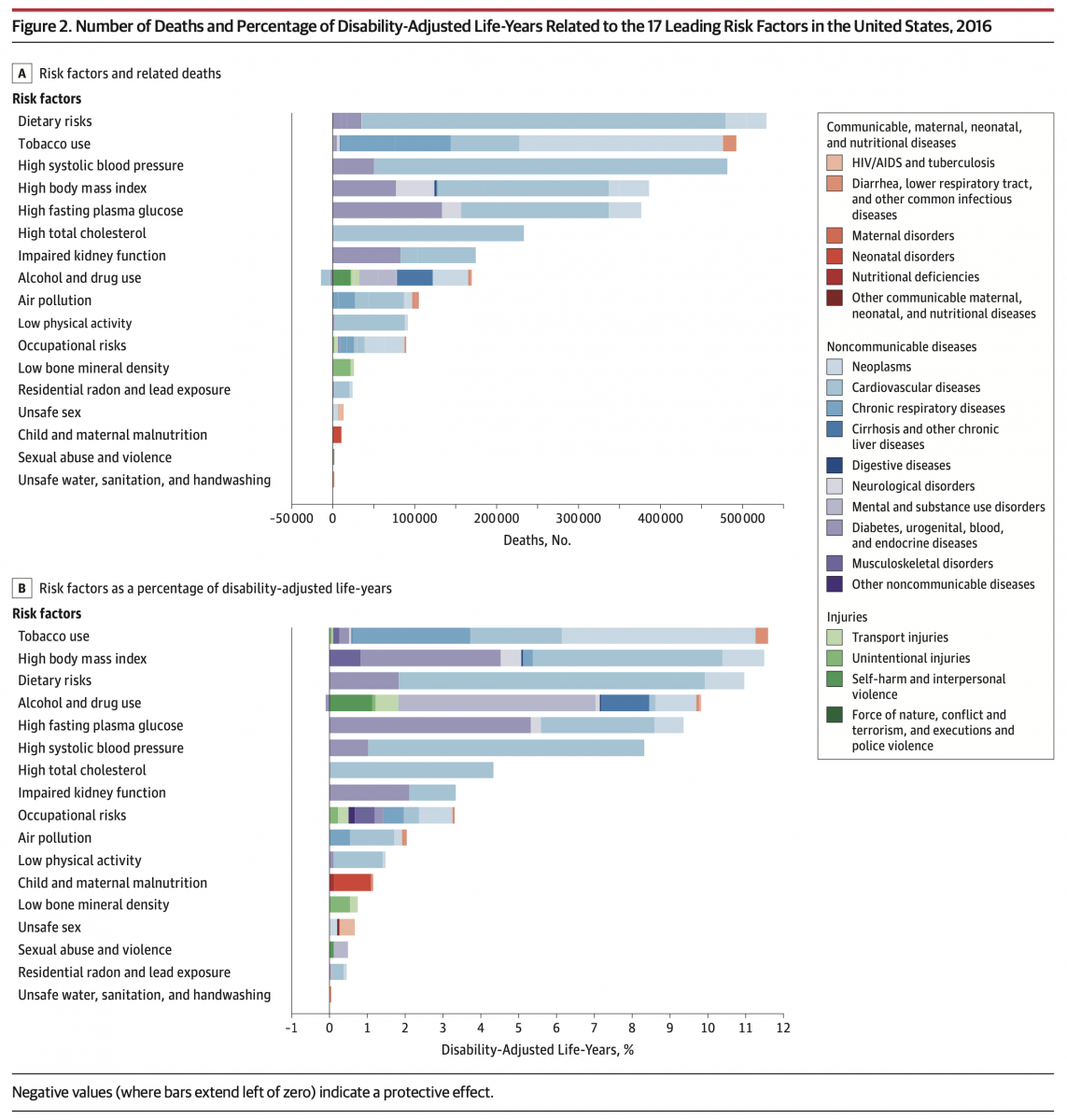
The American health care system must solve the so-called “upstream” biopsychosocial factors that cause ~85% of our health outcomes. We can't keep putting "band-aids" on chronic conditions, while not addressing the root causes. And we need to link preventive public health measures to clinical intervention services through engagement with community-based resources.
Most important, we must create sustainable business models that pay livable wages to exercise physiologists, nutritionists, health educators and health coaches, for theirs is the work that will save America's health and well-being.
- GEMoore
REFERENCES
1) GE Moore, C Carlson, JP Bonnet, EM Phillips, EA Joy, C Collings, W Kraus, WO Roberts. Implementation of Exercise Management Services Among Sports Medicine Physicians in the United States. Clin J Sport Med, February 8, 2024. DOI: 10.1097/JSM.0000000000001209
2) N Elgaddal, EA Kramarow, C Reuben. Physical activity among adults aged 18 and over: United States, 2020. NCHS Data Brief, no 443. Hyattsville, MD: National Center for Health Statistics. 2022. DOI: https://dx.doi.org/10.15620/cdc:120213.
3) The US Burden of Disease Collaborators. The State of US Health, 1990-2016 Burden of Diseases, Injuries, and Risk Factors Among US States. JAMA. 2018;319(14):1444-1472. doi:10.1001/jama.2018.0158
- GE Moore MD's blog
- Log in to post comments
- Follow our Blog
