Ruth Marcus, Associate Editor of The Washington Post, recently wrote an incredibly honest opinion piece about GLP-1 agonists for weight loss. GLP-1 stands for glucagon-like peptide-1, a hormone that regulates glucose metabolism and has many positive effects, improving cardiac, kidney, pancreas, lung and muscle function, as well as bone metabolism, lipid metabolism, and gastrointestinal motility. From a patient’s perspective, however, these medicines suppress hunger.
GLP-1 is in a class of molecules called incretins, which came under intensive research after it was discovered that weight-loss surgery increases GLP-1 after a meal. Marcus quoted Dr. George Bray, a renowned obesity researcher, as saying that GLP-1 agonist drugs are “…the equivalent of bariatric surgery, but without the surgery”. Perhaps more important, the loss of weight and improved metabolism lowers blood lipids, blood pressure and reduces the need for devices to treat sleep apnea.
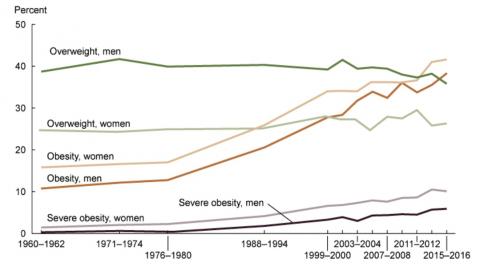
With some 70% of Americans either obese or overweight, 37.3 million (11.3%) having diabetes and another 94 million having prediabetes, many folks are hoping that incretins mark an inflection point in the management of weight-related conditions. People have dreamt for decades of a weight-loss pill, going back nearly 100 years to use of thyroid extract, then 2,4-dinitrophenol, then amphetamines, fen-phen and sibutramine, all of which were discontinued due to adverse side-effects. Knowing this ugly history, some of us are holding our breath on incretins.
In a ‘free market’ economy (which US health care is not), there are a range of ways to price a weight-loss medication. The high-priced easy way would be to set a price against weight loss surgery, something in the range of $10,000-$25,000 . The low-priced but more difficult way, would be to estimate the per-person costs of excess weight. Annual health care costs secondary to excess weight are estimated at $173B (for about 200 million Americans), or about $865 per person / year. Absenteeism costs $79 and presenteeism (being at work but not getting things done) costs $132. All together, a net cost of about $1076 per person / year. Of course, we do not yet know how much society will save because of incretins, which would help offset the costs. Thus, depending on how one wants to market these medications, they could be cost-competitive and fairly priced at something between $1,000 a year and $1,000 a month - which is to say from a lot of money to an awful lot of money.
In fact, Marcus’s prescription cost $1071 a month, of which she only paid a $25 co-pay. Marcus mused that, if incretin analogues are the magic pill to control weight, use of these pills leads to a socio-economic issue. That’s because overweight, obesity and weight-related conditions are skewed to the less well educated and poor. With about 1 in 3 Americans standing to benefit from GLP-1 agonists, how will America pay for incretins when it currently costs nearly $15,000 per person per year? Especially when weight-related conditions are skewed to people who are under-insured and don’t have that kind of cash for medicines.
When a condition rises from afflicting 10-15% of the population (1960) to about 40% of the population 60 years later, that’s an epidemic. The obesity epidemic is slow moving, so it doesn’t get recognized like COVID was, but it’s still an epidemic. Getting swept up in an epidemic is nobody’s fault, it’s not a flaw in their genes, it’s because they were alive at a particular time and place. The main reason we haven’t made progress in curing this epidemic is that we don’t understand why it happened, though most authorities believe it has something about how we live, our lifestyle.
Assuming that today’s incretins aren’t discontinued because of adverse effects, how will that who lifestyle advocates who favor modifying a person’s relationship with his or her environment? There are, in fact, several different approaches (including bariatric surgery, GLP-1 agonists and a number of different diets combined with exercise) that have been proven to achieve a complete remission of type 2 diabetes. Complete remission meaning normal blood glucose measures without any diabetes medications. All those approaches require similar magnitudes of weight loss, nominally 30% or more of body weight.
Sadly, America's focus just on weight is short-sighted. Having a high quality-of-life requires both a sound mind and a sound body, of being able to think for oneself and tend to one’s own needs without assistance. For that, there are no substitutes for mental well-being or for physical strength and endurance. Being a normal weight, by itself, is not enough. All weight loss interventions should be coupled with efforts to improve mental/spiritual peace-of-mind, a healthy social life, better sleep, and improved physical functioning arising from increased strength and endurance. Though if the past is any predictor, I suspect most people will just take the medicine.
Citations
https://www.washingtonpost.com/opinions/2023/06/06/ozempic-weight-loss-ruth-marcus/
https://www.cdc.gov/obesity/basics/consequences.html
- GE Moore MD's blog
- Log in to post comments
- Follow our Blog
