Recently, the Department of Health and Human Services (HHS) issued the 2015-2020 Dietary Guidelines, almost a year after the Advisory Committee submitted its recommendations. These Guidelines are a big step forward, although not as big as many food advocates had hoped for.
The top-level main Guidelines are relatively basic and mundane points. Additional Key Recommendations, an update of old advice from Ancel Keys, are the real substance in these new Guidelines (more on this below). Searching even deeper, one finds HHS hewing to the Advisory Committee’s support for the Mediterranean, vegetarian-style and DASH diets, citing robust evidence that these cuisines reduce cardiovascular disease and improve longevity.
DIET PATTERNS, NOT NUTRIENTS
Dr. Alice Lichtenstein, Vice-Chair of the Advisory Committee, has long promoted cuisines and dietary patterns over the traditional focus on nutrients, and these guidelines are huge step along these lines. Do not underestimate the significance of changing towards a holistic approach to diet (away from reductionism).
Long ago, nutritionists understandably fell into a reductionist molecular model. Insight on the physiologic roles of nutrients led to cures and treatments for scurvy, rickets, beri-beri, and metabolic conditions like gout. Many congenital conditions such as Tay-Sachs and neural tube defects fit well with the molecular model of medicine, in which a single chemical (or just a few) cause disease.
The problem is, outside of diseases of deficiency, piecemeal addition of nutrients just doesn’t produce healthier outcomes. Study after study – vitamin A, vitamin E, vitamin C, fish oils, many others – supplements rarely work and surprisingly often do harm.
The fundamental error in reductionist nutrition for health is the assumption that a specific nutrient is the cause of a particular food’s beneficial effects. The truth is that every food has thousands, if not tens of thousands of compounds, and we only know a few of them. Moreover, in the Mediterranean diet, for example, for all anyone knows the benefit comes from interactions between nutrients when mixing olive oil with garlic, basil and oregano, in a meal combining fish, garden vegetables and red wine.
Complete clarification of food complexity won’t happen in our lifetimes, there are too many variables and unknowns, and the outcomes we’re looking for are driven by highly complex system-level factors and interactions. Accordingly, the substantial step forward in these new Guidelines is the acknowledgement that holistic approaches, not reductionist ones, should drive dietary patterns.
GOOD FOR BUSINESS?
The molecular model has worked well for the processed food industry, which turns raw foods into constituent compounds that become ingredients for what Michael Pollan calls “edible food-like substances”. Achieving much higher profit margins than can be attained by selling raw food, producers combine these ingredients with fat, salt and sugar into tasty and convenient products. That’s good for sales, but bad for America’s waistline, because the combination of fat, salt and sugar is really, really hard to stop eating.
Some critics are disgruntled that HHS didn’t state more clearly that staying under the new limits for sugar and sodium will be very difficult for anyone who eats a standard American diet (SAD) and edible food-like substances. Again, one suspects the influence of food industry lobbyists, since such advice would be bad for their businesses. Many health advocates would prefer a more concise:
“Don’t eat _____”.
In fairness to food producers, they can’t shift abruptly from reductionism to holism, to making products healthier than today’s edible food-like substances. Such change will take time, more than one cycle of Dietary Guidelines, because it requires innovations up and down the product chain, product cycles, investment planning, etc. It likely would not benefit anyone if the Dietary Guidelines got too far out in front of that change. I’m not making excuses for the food industry, but am just imagining why HHS didn’t rubber-stamp the Advisory Committee recommendations.
EGGSACTLY

Newsmedia have noted the shift away from cholesterol molecularism, the focusing of attention on dietary cholesterol in prevention of cardiovascular disease, noting that it’s 'suddenly OK' to eat eggs. Well, in 30 years as a lifestyle physician, I’ve heard no lipidologist nor registered dietitian ever routinely advise against moderate consumption of eggs! My medical school class was fortunate to have a course in human nutrition. Even more fortunate, that class was taught by Drs Michael Brown and Joseph Goldstein, who, when my class was on 3rd-year rotations, won the Nobel Prize for their work on LDL cholesterol receptors. Brown and Goldstein taught us that the liver makes so much cholesterol every day (about 1 gram) that the cholesterol in an egg (about 0.2 grams) doesn’t have significant impact on blood lipid levels in someone with normal liver function.
Patients are often amazed that the real reason to count eggs is that people who eat them for breakfast tend to have them fried in bacon fat, with buttered toast, fried hash browns and bacon or sausage on the side! It’s not about the eggs, except as a marker of SAD cuisine.
EAT WELL AND STAY WELL
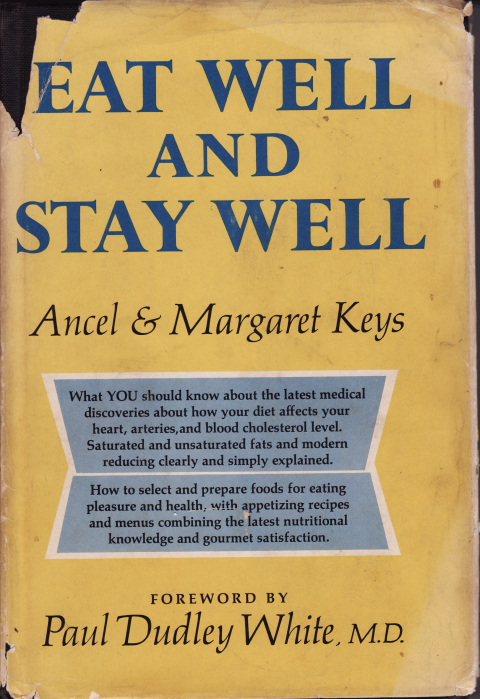
The step forward to an emphasis on dietary patterns is paradoxically a step back to the advice given by Ancel Keys and his nutritionist wife Margaret, in Eat Well and Stay Well, published in 1959. Compare the new Key Recommendations to what the Keys wrote on page 40 of their book:
Summing up, here is our best advice:
1. Do not get fat; if you are fat, reduce.
2. Restrict saturated fats, the fats in beef, pork, lamb, sausages, margarine, solid shortenings, fats in dairy products.
3. Prefer vegetable oils to solid fats, but keep total fats under 30 per cent of your diet calories.
4. Favor fresh vegetables, fruits and non-fat milk products.
5. Avoid heavy use of salt and refined sugar.
6. Good diets to not depend on drugs and fancy preparations.
7. Get plenty of exercise and outdoor recreation.
8. Be sensible about cigarettes, alcohol, excitement, business strain.
9. See your doctor regularly and do not worry.
Anyone who has followed the Keys’s advice (for up to 57 years) should probably just keep doing what they’ve been doing.
Minor differences between the Keys and the new Guidelines are:
- The Keys advised an upper limit of 30% of calories from fat, the new Guidelines don’t specify an upper limit and recommend <10% of calories from saturated fats;
- The Keys didn’t define “heavy use” of salt and sugar, while the new Guidelines specifies an upper limit of 2300 mg sodium and 10% of calories from added sugars;
- The Keys didn’t define “sensible” alcohol consumption, the new Guidelines specify 1 drink per day for women and 2 drinks per day for men;
- The Dietary Guidelines explicity support whole grains, legumes, nuts, and soy products, while the Keys didn’t mention these foods in their 9-point advice, they were discussed many other times in the book; and
- The Dietary Guidelines explicity discourage trans fats, the Keys did so indirectly in advising against margarine and solid shortenings (i.e., hydrogenated oils).
Of course, the HHS evidence-based recommendation on the Mediterranean diet rests primarily on the PREDIMED trial - a randomized trial based on epidemiology by Ancel Keys in the Seven Country Study. PREDIMED proved that the Mediterranean diet prevents cardiovascular disease.
EXERCISE & ENTANGLEMENT
Some commentators have complained about HHS linking the new Dietary Guidelines to the HHS Physical Activity Guidelines, criticism that is unwarranted.
Overweight affects ⅓ of Americans, obesity another ⅓, diabetes 1-in-10, pre-diabetes probably another 2- or 3-in-10, and only ¼ of Americans meet the Physical Activity Guidelines. With America in this situation, the entanglement of diet and exercise should not be compartmentalized. Exercise alone doesn’t usually produce substantial weight loss, but exercise is immensely important in reducing abdominal fat, improving skeletal muscle metabolism of fat and glucose, and preventing weight gain.
The Keys recommended almost twice as much exercise as the current Physical Activity Guidelines, and even specified outdoor recreation. Indeed, if low vitamin D levels are a concern, Americans probably should do more outdoor activities! The Keys also mentioned stress, anxiety and - years before the US Surgeon General - implied that smoking is harmful to health.
The new Dietary Guidelines have a substantial section, written more for public health and policy advocates, that discusses health ecology issues such as availability of produce and fresh foods and the impact of socio-economics. Perhaps the 2020-2025 Dietary Guidelines will delve further into non-food issues that affect many people’s diet.
Americans feel they don’t have the time, money or energy to spend on better nutrition and physical activity. Whether it’s driving their kids to extra-curricular activities, paying for car or mortgage or student loan payments, working a second job, caring for elderly family members, or a long list of other over-commitments…whatever the reasons, diet and exercise just aren’t top priorities for many, many people.
In the 57 years since Eat Well and Stay Well was published, Americans have moved away from heartland farm communities to coastal cities. Today, both Dads and Moms go to work, causing real family challenges with shopping for food, preparing meals, and dining as a family. Fewer and fewer Americans still live as life was portrayed in Leave It to Beaver.
Vast numbers of Americans live disconnected from food sources. Grocery stores grow larger and larger and few people still go to small or local grocers, butchers and bakers. We favor convenience cuisine, premade meals or something ready-to-eat after a few minutes in a microwave oven. Despite concerns over landfill costs from the disposable packaging, we’re glad there’s little time spent cleaning up the kitchen so that we can get to ________.
This shift towards convenience cuisine has coincided with home-building in the suburbs and exurbs, where planners assume everyone drives to Big Box stores every 1 or 2 weeks, filling SUVs with edible food-like substances because they have good shelf-life. The roads and highways favor motor vehicles, not pedestrians or cyclists, discouraging active transportation.
Some Americans respond to these shifts by joining a gym, but many people just don’t identify with that. Strengthening and conditioning feel more like a chore than recreation, less the means to a goal and more of an end in itself. Personal trainers and exercise device makers counter this aspect of gyms, by “game-ifying” gym activities. In today’s urban and suburban communities, it can be challenging to maintain physical fitness for someone who doesn’t like going to a gym.
BACK TO THE FUTURE
American health care is steeped in reductionism, dominated by specialists skilled with procedures and exotic drugs. The Keys advised that healthy diets “do not depend on drugs and fancy preparations”, but the American College of Cardiology and American Heart Association advocate a prevention model that would put about 1-in-7 people on a statin.
The major burdens of disease of today - overweight, obesity, heart disease, diabetes, arthritis, back pain, depression, anxiety, cognitive decline - are not caused by single-molecule flaws in metabolism. They’re the result of integrative biology, driven most strongly by social, behavioral, economic and environmental factors - we are what we eat, what we do, what happens around us.
Modern social forces undermine healthy choices. American life amplifies stress and causes us to compensate with convenience cuisine, consuming edible food-like substances while staring a screen of pixels. Many people, mired deep in that predicament, find that un-entangling oneself is very much more difficult than it sounds. No guideline, no analysis of Big Data, no quantifying of oneself with wearables, nor even behavioral counseling “get activated” are sufficient to dig America out of our health ecology quagmire. It’s going to take all of those and - most important - a restructuring of our social fabric so that Americans find it difficult to not be active, eat well and be well.
The new HHS Dietary Guidelines, revisiting and updating old wisdom, provide a step in the right direction.
Now we need to get Congress to fund an update of the Physical Activity Guidelines as well.
SUGGESTED READINGS
U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015 – 2020 Dietary Guidelines for Americans. 8th Edition. December 2015. Available at http://health.gov/dietaryguidelines/2015/guidelines/.
Ramón Estruch, Emilio Ros, Jordi Salas-Salvadó, et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N Engl J Med 2013; 368:1279-1290. DOI: 10.1056/NEJMoa1200303
David A Kessler. The End of Overeating. Rodale Press, Emmaus, Pennsylvania, 2009.
Ancel & Margaret Keys. Eat Well and Stay Well. Doubleday, New York, 1959.
Marion Nestle. Food Politics. University of California Press, Berkeley, 2002.
Michael Pollan. The Omnivore's Dilemma. Penguin, New York, 2006.
Michael Pollan. In Defense of Food: An Eater's Manifesto. Penguin, New York, 2008.
- GE Moore MD's blog
- Log in to post comments
- Follow our Blog
